What is A1AT Deficiency? A Look at the Genetics
This guide will walk you through what A1AT Deficiency is, its symptoms, how it’s diagnosed, and the available treatment options to help you or a loved one navigate this complex condition.
What is A1AT Deficiency? A Look at the Genetics
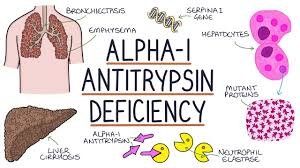
At its core, A1AT Deficiency is a genetic disorder. Our bodies produce a protein called Alpha-1 Antitrypsin (A1AT) primarily in the liver. The main job of this protein is to travel to the lungs and protect them from damage caused by inflammation and irritants, especially from an enzyme called neutrophil elastase.
In people with A1AT Deficiency, a faulty gene (the SERPINA1 gene) causes two main problems:
- Not enough A1AT protein reaches the lungs: Without this protective shield, the lungs are vulnerable to damage, which can lead to conditions like Chronic Obstructive Pulmonary Disease (COPD) or emphysema, often at a much younger age than typical.
- A buildup of abnormal A1AT protein in the liver: The misfolded, abnormal A1AT protein gets trapped in the liver cells where it’s made. This buildup can cause liver damage, scarring (cirrhosis), and an increased risk of liver cancer.
Recognizing the Symptoms of A1AT Deficiency
Because it affects two different major organs, the symptoms of A1AT Deficiency can vary. It’s crucial to know what to look for, as early diagnosis can make a significant difference in outcomes.
Lung-Related Symptoms
Lung problems usually appear in adulthood, typically between the ages of 20 and 50. Smokers with A1AT Deficiency tend to develop symptoms much earlier and more severely. Key signs include:
- Shortness of breath, especially during physical activity
- Chronic cough, with or without phlegm production
- Wheezing or a whistling sound when breathing
- Recurring chest colds or respiratory infections
- A diagnosis of COPD, emphysema, or chronic bronchitis, particularly if you’re under 45 or have no history of smoking
- Decreased ability to exercise
Liver-Related Symptoms
Liver issues can appear at any age, from infancy to adulthood. In newborns, it can be a cause of jaundice. In adults, the signs might be more subtle at first.
- Unexplained elevated liver enzymes on a blood test
- Fatigue and weakness
- Swelling in the legs or abdomen (edema and ascites)
- Jaundice (yellowing of the skin and eyes)
- Enlarged spleen
How is A1AT Deficiency Diagnosed?
If you or your doctor suspect A1AT Deficiency based on your symptoms or family history, diagnosis is straightforward. It usually involves a simple two-step process:
- A1AT Level Test: A simple blood test measures the amount of A1AT protein in your bloodstream. If the levels are lower than normal, it points towards a potential deficiency.
- Genotype Test: A second blood test or a cheek swab is used for genetic testing. This test confirms the diagnosis by identifying the specific faulty genes you carry.
The World Health Organization (WHO) recommends testing for A1AT Deficiency in all patients with COPD, unexplained liver disease, and adults with asthma that doesn’t respond well to treatment.
Treatment and Management Strategies for A1AT Deficiency
While there is no cure for A1AT Deficiency, there are effective ways to manage the condition, slow its progression, and improve quality of life.
1. Lifestyle is Key
- DO NOT SMOKE: This is the single most important step for anyone with A1AT Deficiency. Smoking drastically accelerates lung damage. Avoiding secondhand smoke is also crucial.
- Protect Your Lungs: Avoid exposure to dust, fumes, and other environmental pollutants.
- Stay Active: Regular exercise, as tolerated, can help improve lung function and overall health.
- Get Vaccinated: Annual flu shots and pneumonia vaccines are essential to prevent respiratory infections that can cause further lung damage.
2. Medical Treatments
- Standard Lung Therapies: Patients with lung symptoms are often treated with standard COPD medications, such as inhalers (bronchodilators) and, if needed, supplemental oxygen.
- Augmentation Therapy: For individuals with established lung disease (emphysema) due to A1AT Deficiency, this therapy involves regular intravenous (IV) infusions of A1AT protein collected from healthy plasma donors. This treatment increases the level of the protective protein in the lungs, helping to slow down the progression of lung damage.
- Liver Disease Management: There is no specific treatment to stop the liver damage besides managing the symptoms and complications. In cases of severe liver failure, a liver transplant may be the only option. A successful transplant cures the A1AT Deficiency because the new liver produces normal A1AT protein.
Living with A1AT Deficiency: A Path Forward
Receiving a diagnosis of A1AT Deficiency can be daunting, but it’s also the first step toward taking control of your health. With early diagnosis, proactive lifestyle changes, and appropriate medical care, many people live full and active lives.
If you have symptoms of COPD, especially at a young age, or have unexplained liver problems, don’t hesitate. Talk to your doctor about getting tested for A1AT Deficiency. Knowledge is power, and in this case, it’s the power to protect your lungs and liver for years to come.